ABSTRACT
This prospective cohort study evaluated virtual reality (VR) use during outpatient hysteroscopy in a UK tertiary hospital (Nov 2022-Apr 2023). Of 105 eligible women, 38 (36.2%) used VR; most who declined preferred to remain undistracted. Mean pain score was 5.5, slightly lower than the expected 5.7. Mild side effects included dizziness and claustrophobia. Nearly all users (94.7%) would recommend VR, and all rated it “acceptable” or “very acceptable.” While VR may improve patient experience, limited uptake highlights the importance of tailoring pain management to individual preferences.
Introduction
Hysteroscopy is a key intervention used within gynaecology1,2, which can be completed in an outpatient setting3 without needing general anaesthesia or an operating theatre. This provides several benefits to both patient and healthcare system: shorter recovery time, lower complication rates, reduced costs, increased convenience, and the potential for a “see-and-treat” approach.4-8 However, pain has been cited as the most common reason for a failed outpatient hysteroscopy (OPH) procedure, and it is known that up to a third of patients will experience “severe” pain during such procedures.6, 8
The increasing use of technology within healthcare has propelled virtual reality (VR) forward as a potential distraction technique to reduce pain perception.9 There has been an interest in the use of VR as a non-pharmacological pain relief option in OPH to improve patient experience. Indeed, there have been a few randomised controlled trials (RCTs) assessing the use of VR during OPH for pain management.10-15 A meta-analysis in 2023 concluded that VR does not decrease pain during office-based hysteroscopy, but it may reduce anxiety.16 However, the meta-analysis highlighted several limitations, including the relatively small number of patients evaluated thus far using VR during OPH.
We conducted a prospective observational study to evaluate the uptake, acceptability and effectiveness of VR for pain control in routine OPH clinics for both diagnostic and operative procedures.
Methods
Study Design
An uncontrolled, prospective observational cohort study in a single tertiary specialist National Health Service Hospital in Birmingham, UK was conducted between November 2022 and April 2023 to evaluate the acceptability of VR headsets during OPH and other intrauterine procedures and their efficacy for controlling pain. Local Institutional Review Board approval was gained for a quality improvement project (CARMS-31988). VR headsets were provided by SyncVR Medical (https://www.syncvrmedical.com/) and controlled by a healthcare assistant supporting the patient. The patient could choose between a variety of relaxing virtual environments or a guided breathing/relaxation session. The sound from the simulated environment was played aloud in the room or on headphones, depending on the patient’s preference of having a fully immersive experience. The headset and headphones were sanitised (in accordance with infection control policies) between patients using disposable alcohol wipes. 3.1 mm diameter hysteroscopes (Karl Storz, Germany) were used for most procedures, apart from hysteroscopic polypectomies, which were performed using 5.0 mm hysteroscopes (TruClearTM 5C Hysteroscope Set, Medtronic, US).
Participants
A poster advertised VR use in the clinic waiting area (Supplementary Questionnaire 1). Women aged 18 and over attending for elective intrauterine procedures were eligible; those with limited English comprehension were excluded.
Consenting women completed a pre-procedure questionnaire including demographic data (Supplementary Questionnaire 2). A clinician questionnaire captured VR uptake and reasons for refusal (Supplementary Questionnaire 3).
Outcomes
The primary outcome was pain experienced during the procedure on a 10 cm visual analogue scale (VAS) ranging from 0 (no pain) to 10 (worst pain imaginable) (Supplementary Questionnaire 4). This was completed in the immediate post-operative period when the patient was reviewed. Women were asked to complete the VAS and indicate the amount of pain they expected to experience as well as their current level of anxiety, ranging from 0 (no anxiety) to 10 (worst imaginable anxiety), before the procedure (Supplementary Questionnaire 2). Secondary patient-centred outcomes were collected in the post-procedure questionnaire (Supplementary Questionnaire 4). This included the overall experience using a 5-point Likert scale (“very acceptable”; “acceptable”, “neither acceptable nor unacceptable”; “unacceptable” and “very unacceptable”), whether patients would recommend undergoing this procedure using VR, whether the use of VR headset was partial or throughout the procedure and any side effects experienced. Patients also had an opportunity to provide additional feedback through free-text comments.
The use of any pre-procedural analgesia was documented along with its timing, and any additional analgesia provided was recorded by the clinician (Supplementary Questionnaires 2 and 3).
Statistical Analysis
Descriptive statistics were used. Dichotomous outcomes were reported as counts and percentages; continuous outcomes as means with 95% confidence intervals (CI). For pain analysis, combined procedures were ranked hierarchically by typical pain intensity: endometrial polypectomy > coil insertion/change > blind Pipelle® endometrial biopsy > directed Pipelle® biopsy > diagnostic OPH > cervical polypectomy, based upon published procedural pain data.8, 17 All statistical analysis was performed using SPSS software version 29 (IBM, Armonk, USA).
Results
Out of 105 eligible women approached during the study, 38 (36.2%) women agreed to participate and use VR headsets during their procedures. Figure 1 shows a list of reasons for declining the use of VR headsets.
The mean age of the participants was 48.6 years (range: 29-75 years old). The ethnicity spread was representative of the local population [ethnicity: White 55.3% (48.6%); Asian 31.6% (31.0%), and Black 13.2% (10.9%)].18 36.8% (n=14) of the participating women were post-menopausal and 57.9% (n=22) had a history of vaginal delivery. Participants underwent a variety of procedures, ranging from OPH (n=36, 94.7%), Pipelle® (Cooper Surgical, CA, USA) endometrial biopsy (n=18, 47.4%), polypectomy using a hysteroscopic tissue removal system (Truclear® Office 5C, Medtronic, MI, USA) (n=4, 10.5%), coil insertion/change (n=7, 18.4%), directed hysteroscopic biopsy (n=2, 5.3%) and cervical polypectomy (n=1, 2.6%).
Eighteen participants had some form of analgesia before or during the procedure (47.4%), with a median time of 60 minutes pre-procedure (range: 0-360 minutes). This included paracetamol, non-steroidal anti-inflammatory drugs, co-codamol, codeine phosphate and tramadol. Two women (5.3%) had an intracervical local anaesthetic block during their procedure, and one woman (2.6%) required inhalational analgesia in the form of Entonox®.
The overall mean pain score experienced was 5.5 (95% CI: 4.5–6.1) [standard deviation (SD): 2.8] which was lower than the mean expected pain score of 5.7 (95% CI: 5.0–6.5) (SD: 2.2). The mean level of anxiety before the procedure was 5.3 (95% CI: 4.5–6.1) (SD: 2.4). The most painful procedure in this cohort was a directed hysteroscopic biopsy and the least painful procedure was a cervical polypectomy (Table 1).
Mild side effects were reported by three women (7.9%); two reported claustrophobia, and one reported dizziness. Six women (15.8%) used a VR headset during part of their procedure only, with three wanting to see what was going on and not be distracted. Other reasons for stopping included anxiety (n=2) and the use of Entonox® (n=1). The majority of participants would recommend undergoing their procedure using VR (n=36, 94.7%), and all women rated their procedure as either “acceptable” or “very acceptable” (n=38, 100%).
Discussion
Principal Findings
All the patients who used VR headsets found them acceptable during OPH and other intrauterine procedures, with less than one in ten reporting some mild side effects. However, only a third of women were willing to use VR during their procedure. Of those that did, almost one in five discontinued their use. Half of those declining VR stated that they wanted to see what was going on and not be distracted, and this was also the main reason for discontinuation. The average pain experienced was marginally less than the pain patients expected and in keeping with published data.8 The vast majority of women who used VR recommended its use for undergoing common OPH or intrauterine procedures.
Strengths and Limitations
In this study, we assessed pain using an assessment scale which is validated to assess acute pain.19, 20 We also explored the utility and side effects of using VR in an outpatient gynaecology setting with no missing outcome data. This was not a randomised study, and the absence of a control group limits the strength of the conclusions. The small number of participants who used VR further limits the reliability of the findings. Due to this small study size and the lack of a control group, reliable comparative analysis between procedures was not possible, nor was the ability to make strong inferences for clinical practice. However, we believe that our data collected from a routine clinical setting is generalisable and adds to the overall data accumulating from observational and experimental studies evaluating the use of VR for gynaecological procedures like hysteroscopy.
Comparison with Existing Literature
A review of the existing literature identified six RCTs involving the use of VR in OPH. One of those trials was a conference abstract reporting an analysis of the preliminary results and included only a quarter of the intended sample size.11 The five other RCTs looking at the use of VR for pain scores during hysteroscopy reported variable and conflicting findings.10, 12-15 Three also looked at the associated anxiety levels of the patient.10, 13, 15
A systematic review and meta-analysis by Cohen et al.16 in 2024 included four of these six RCTs10, 12, 14, 15 and showed that intraprocedural pain score was not improved by the use of VR, but there was a reduction in anxiety levels during OPH. A more recent systematic review with meta-analysis included two additional RCTs involving a total of 457 patients. In contrast, they found that VR was associated with a significant reduction in pain score during the procedure compared to the control group [mean difference (MD): -1.43, 95% CI, P<0.001).21 There was also a significant decrease in anxiety (P=0.01) and the pain score post-procedure (MD: -1.52, 95% CI, P<0.001) in the VR group.21
Inferences from these meta-analyses are limited by relatively small samples, differences in the VR equipment used, VR environment video, types of hysteroscopes, other analgesia provided, as well as different pain measurement scoring systems. Future research should look at the type of VR technology used, the context where it is deployed and for what kind of procedure.
Implications for Clinical Practice
While most users found VR acceptable and would recommend it for hysteroscopy and intrauterine procedures, its utility for short procedures appears limited. In our study, two-thirds of women declined its use to aid pain control. This proportion is higher than the first RCT evaluating VR for OPH, where only 6/53 (11%) declined to use VR.10 The observation from our study, performed in a routine, day-to-day clinical setting, gives an insight into the willingness of the typical woman attending the ambulatory gynaecology setting to use VR. The low uptake is likely to impact the cost-effectiveness of utilising VR technology in this setting. The target procedures in our study were short but intimate examinations by nature, necessitating continuous two-way communication between the clinician and conscious patient for reassurance and information-giving. This communication is disrupted by the use of VR headsets, and the desire to no longer be distracted was the main reason for discontinuation in those initially using VR. Cheaper, more individualised alternatives such as listening to music or looking at a relaxing landscape on the ceiling, while not fully immersive, may be simpler and more cost-effective distraction techniques for short, common intimate procedures.
Conclusion
The provision of adequate analgesia in the outpatient setting for hysteroscopy and other intrauterine procedures remains a challenge, and it is often a case of taking a tailored approach to each patient. While VR is an emerging medical tool, its place and usefulness in ambulatory gynaecology are yet to be determined.
Acknowledgements
References
Suplementary Materials
Supplementary Figure 1
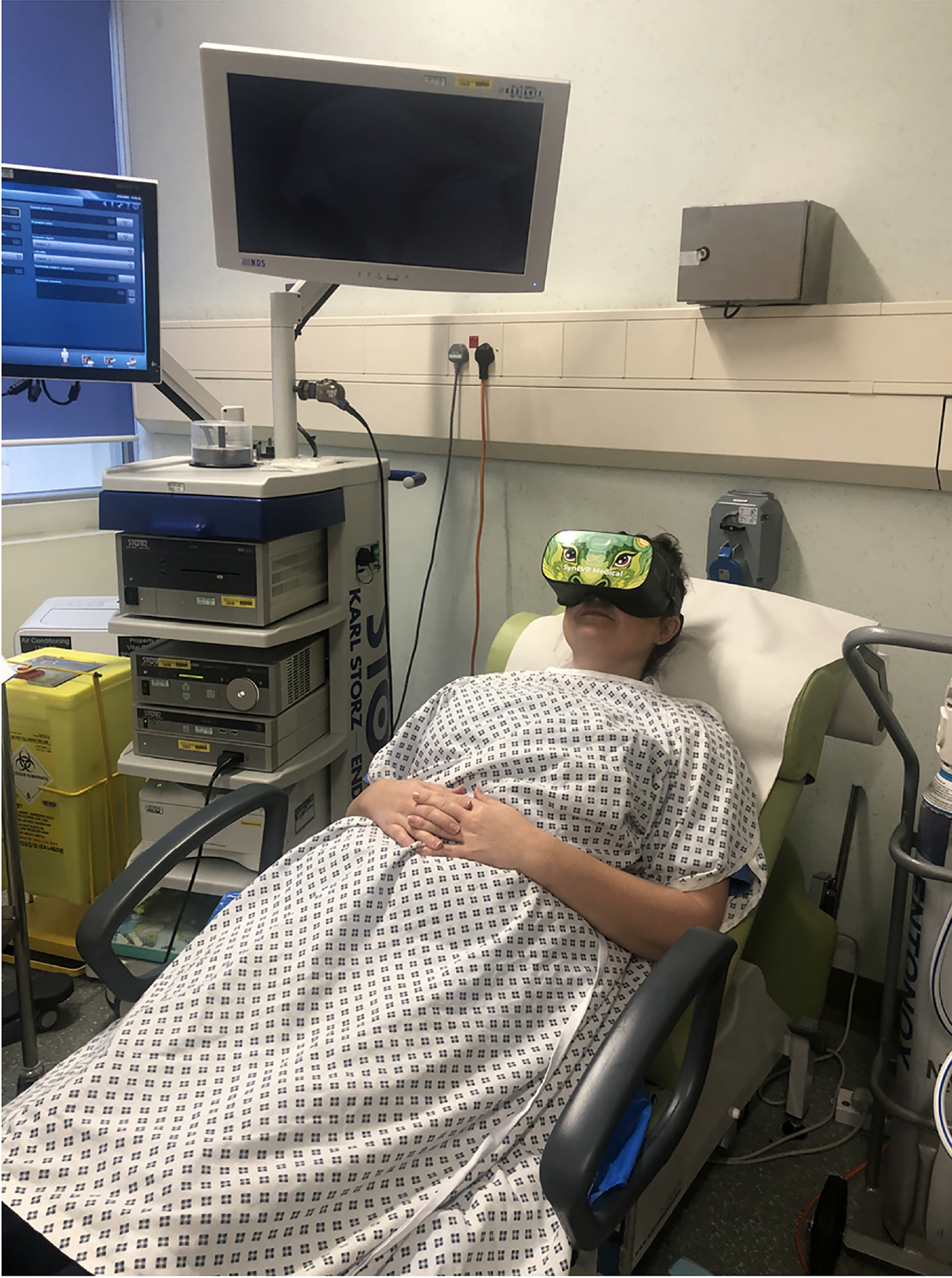
Virtual reality in outpatient hysteroscopy. We are currently trialling virtual reality headsets in outpatient hysteroscopy to see if it improves your experience. Please speak to your doctor/nurse if you want more information or if you would like to try them during your appointment.